Published on the 8th June 2018 by ANSTO Staff
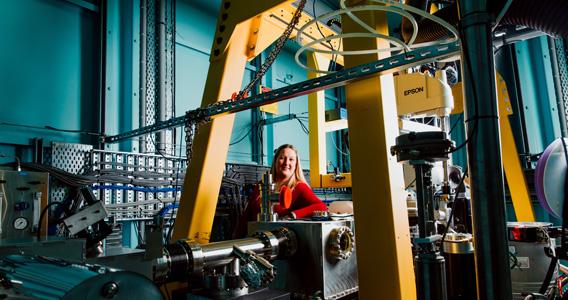
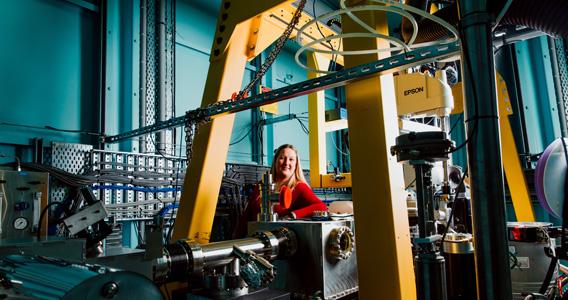
Associate Professor Stephanie Gras at the Australian Synchrotron
While treatments for HIV mean that the disease is no longer largely fatal, the world still lacks a true therapy that can eradicate the virus across a globally – and genetically different – population.
Monash researchers, together with colleagues from the Pasteur Institute in Paris, have discovered a unique set of “super” receptors on immune cells capable of killing HIV across genetically diverse populations, making them a potential candidate for immunotherapy treatments. The work was recently published in Science Immunology.
Associate Professor Stephanie Gras and her team from the Monash University Biomedicine Discovery Institute and ARC Centre of Advanced Molecular Imaging, and her colleagues from the Pasteur Institute in Paris, studied fifteen unique individuals who all had been infected with HIV (ANRS CO21 CODEX cohort), but have immune system that protect them from AIDs progression. These rare individuals, called HIV controllers, could hold clues to the cure for the disease.
Upon HIV infection, CD4 T cells, which are an important part of our protective immune system, can be depleted and drop dramatically in numbers, leading to a weak immune system with the progression of the disease to AIDs. These CD4 T cells can remain low even when the disease is kept in check with anti-retroviral therapy (ART), which is currently provided to more than half of people living with HIV globally. ART lowers the risk of mortality but does not eradicate the virus.
Associate Professor Gras and her colleagues found that HIV controllers are able to retain CD4 T cells of a higher quality, able to detect and react to minute amounts of virus, therefore representing a great opportunity to study their potential role in HIV infection.
We discovered that those CD4 T cells, usually viewed as helper cells for the killer CD8 T cells that destroy infected cells, could be turned into killer cells themselves in HIV controllers. These killer CD4+ T cells could recognize very low amounts of HIV thanks to the expression of “super” T cell receptors on their surface. Importantly when they studied these receptors – they found identical receptors across multiple HIV controllers. “The likelihood of finding the exact same T cell receptor in different individuals is extremely low, like winning the lottery, and is likely playing a role in the control of HIV” Carine Farenc, a lead author of the study said.
T cell receptors recognize virus or bacteria fragments bound to specialized molecule called HLA (Human Leukocyte Antigen). HLA molecules are like fingerprints: every person has a specific combination of HLA molecules, which help the immune system recognize foreign invaders like bacteria or viruses.
Monash University researchers used the Australian Synchrotron, effectively a giant microscope the size of a football field, to study the binding of this super T cell receptor in complex with the HIV antigen.
“I looked at the T-cell receptor or TCR and how the TCR is able to recognise the HIV peptide. When we get infected with the HIV virus, the virus will break down into small pieces, peptides, and the peptide will be loaded on to HLA molecule. The HLA molecule is able to present small antigen to the T cell receptor. So using MX1 and MX2, we have been able to look at the interaction between the TCR and the HIV peptide presented by the HLA molecule," said Associate Professor Gras.
“And there is something quite remarkable about our TCR, in that this TCR is able to recognise the same HIV peptide presented by different HLA molecules. HLA molecule is like a fingerprint, we all have different HLA molecules. Each is quite unique. Usually one TCR recognises the HLA molecule but this TCR that we found is able to recognise a lot of different molecules. And using the synchrotron we were able to understand how this was done by the TCR. “
The Gras team and her colleagues found that these killer CD4 T cells can bind with HLA molecules shared by a quarter of world population, a figure that is likely to increase as studies progress, according to Associate Professor Gras.
http://immunology.sciencemag.org/content/3/24/eaat0687
Statistics (from WHO):
In 2016:
- there were 36.7 million people living with HIV
- 1 million died from the disease
- 19.5 million people living with HIV were receiving antiretroviral treatment (ART)
Content provided by Monash University