Neutron capture enhanced particle therapy (NCEPT)
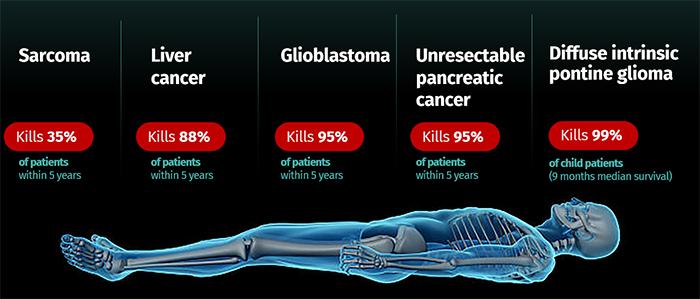
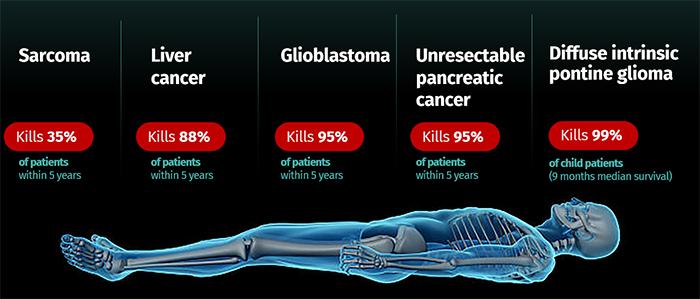
Neutron capture enhanced particle therapy (NCEPT) is a groundbreaking targeted radiotherapy technique pioneered by a multi-disciplinary team at ANSTO and its partner organisations. This innovative approach aims to treat cancers with poor prognosis, including brain cancer, pancreatic cancer and secondary melanoma. NCEPT enhances the effectiveness of particle therapy by combining the primary radiation beam (a proton or carbon ion beam) with a tumour-targeting neutron capture agent, which selectively boosts the radiation dose to cancer cells while minimising damage to healthy tissues.
ANSTO’s sovereign capabilities, including accelerators, neutron and photon sources and imaging technology along with expertise in imaging, particle physics, radiobiology, radiochemistry and therapeutics are crucial to the development and advancement of NCEPT.
By increasing the effectiveness of particle therapy, NCEPT has the potential to shortens treatment times, enabling healthcare providers to treat more patients and optimise the use of limited treatment facilities and resources. This could lead to lower costs per patient for the public health system.
NCEPT offers direct benefits to patients, especially children, by providing more effective radiotherapy through targeted radiation enhancement). This approach aims to reduce debilitating side-effects and late term complications associated with conventional radiotherapy.
Neutron capture enhanced particle therapy: An explainer
Watch the video
The Science
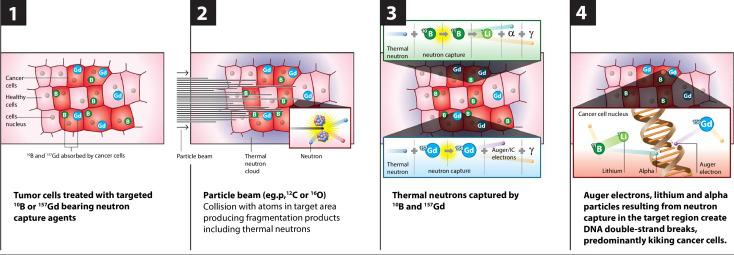
NCEPT delivers a two-pronged attack on cancer cells by harnessing the thermal neutron field that is generated in the treatment area during particle therapy. This process involves capturing these neutrons using tumour-specific neutron capture agents that are biochemically targeted to cancer cells. This results in a radiation dose boost delivered directly to tumour cells - even those outside the primary target area.
The radiobiological dose delivered to the target cancer cells in NCEPT consists of two principal components: the ion dose and the neutron capture dose. ANSTO researchers have shown that this combination enhances the biological effectiveness of the ion beam, either by increasing the tumour dose or allowing the primary beam dose to be reduced which minimises the impact on healthy tissue.
Future directions and clinical translation
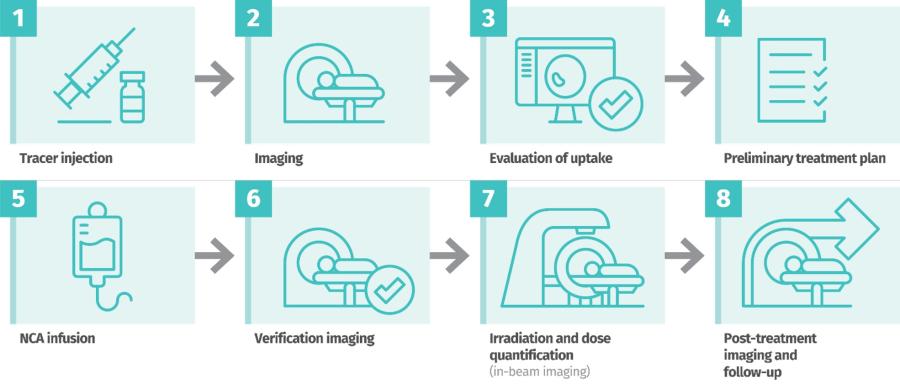
The clinical translation of NCEPT will involve a comprehensive pipeline, beginning with diagnostic imaging using PET and diagnostic analogues of the neutron capture agent to evaluate patient suitability and optimise treatment planning. Following the administration of the therapeutic agent and verification imaging with MRI or PET, patients will undergo irradiation with proton or heavy ion beams, accompanied by real-time dosimetry. Post-treatment monitoring will include follow-up imaging and clinical assessments.
The development of novel tumor-specific and receptor-mediated neutron capture agents, along with their diagnostic analogs, will be crucial to harness the true potential of NCEPT. These advanced agents will enable precise targeting of tumor cells while sparing healthy tissues, thereby enhancing the therapeutic index of NCEPT. Ultimately, carefully designed clinical trials will be necessary to establish the safety and efficacy of NCEPT in cancer patients and pave the way for its integration into the arsenal of advanced radiation oncology techniques.
For more information

